Follow me on my daughter's journey to recovery after a sudden medically unexplained hypoxic brain injury, her 16 months of recovery, and her sudden cardiac arrest that eventually took her life. This is about my beloved Brenna and a mother's reflections while she was ill and after her loss. God has sent me on a journey to use her story to help and educate others. The opinions on this blog are based on 6000 hours spent with My Brenna over a 16 month period.
Playing Dress Up

Brenna wearing Mama's hat.
Tuesday, July 31, 2012
Do you see what I can't see?
Ten months ago on September 26, 2011, shortly after midnight, I noticed Brenna looking around the room. She had a smile on her face and both eyes were open in wonder. Her left eye had been damaged during constant doses of an eye medicine that left her eye not only brown, but looking like a hard fried egg. I hadn't seen both eyes open and looking around for ever so long. This time was different. I could see her rosebud mouth moving as if talking to someone. Her smile was bright and happy. I could see nothing.
I crawled into her bed, cuddled her close to me and asked, "Brenna, what do you see?"
She smiled.
"Brenna, do you see something Mama can't see?"
She just kept smiling.
I held her close and sang the songs God had given me over those months of her illness. Brenna still looked around with her big smile.
Whatever she saw, whomever she was talking to, was someone I could neither see nor hear. I believe her experience was real.
I stayed at her side until her eyes closed and she went to sleep.
When morning came, and I prepared her for the day, her blood glucose counts were normal for the second day in a row. No need to use the "R" insulin. All her body functions were becoming predictable and back to normal. I told her how very proud I was of her progress.
Later in the morning, I worked with her on saying "AH!" She smiled at me and then I heard, "AH!" That was the last picture I have of her. Proudly saying "AH!"
That afternoon, while I went for supplies and left her with a friend, my beloved daughter had a Sudden Cardiac Arrest.
Through the next few days, I retained my routine of caring for Brenna, this time in the ICU of St. Alphonsus Regional Medical Center. The staff was good to her, they were good to me. I curled up in the recliner in the room and waited, waited for my daughter to return to me, one more time.
I prayed to see Brenna open her beautiful blue eyes again. Smile at me again. I just knew that my voice could reach into her being and bring her back to me, one more time. I did not want our journey to be over.
Brenna's coming back this time was not meant to be. On October 1st, I brought her home the last time. I saw the tears in the eyes of the EMTs. In all those months, they had taken her on other trips across town. They knew this was Brenna's last ride in an ambulance. In my heart, I knew my daughter was gone, but my mind did not want to accept.
I cherish the moments, every one I had with her. I have no regrets at saving her life. I have no regrets for the hours and days I spent with her. I loved her before she was born. I loved her all her life. I will love her still, all the days of my life.
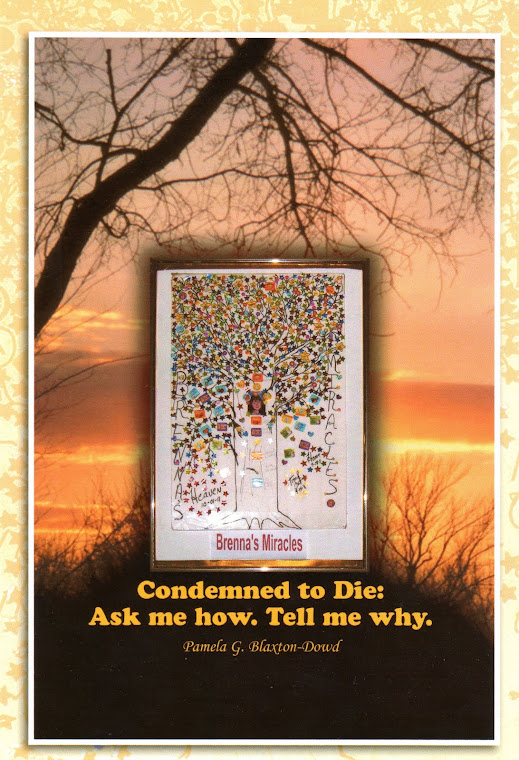
Please read her journey through her fight to recover from her anoxic brain injury. Condemned to Die: Ask me how. Tell me why. Available at Amazon and Barnes & Noble.
Monday, July 30, 2012
No more, "I'll know when I get there."
For a long time, Brenna and I had planned to leave Idaho, but events happened to get in the way. In 2008, we left Idaho and headed to MO, hoping the house would sell and we could find a place there. By the time we arrived in MO, the bottom had fallen out of everything. Nothing was selling and prices had drastically fallen.
While gone, we were in an accident that totalled the pickup and left Brenna with a detached retina in the left eye. That was the beginning of the spiral downhill for her.
My little girl suffered an anoxic brain injury on May 26, 2010. I planned for her to get better. I was still going to take her where she wanted to go. She had chosen a place in Honey Grove, TX to live. It was big enough for rehab equipment and I wanted to have her in a large enough space to teach her to walk again. We had dreams.
Alas, it wasn't meant to be. On October 1, 2011, my little girl died, leaving behind a broken-hearted, restless mother. Without Brenna, I just didn't want to be here. I wanted to move...some place...any place east of here. I didn't really know where I wanted to be, just somewhere but here.
I searched for homes in Oklahoma, to be centrally located in the US, to fly to anywhere I wanted to go. No matter where I contacted a realtor, nothing happened. Realtors either didn't contact me back or I believe they had another agenda on repo homes. I checked out homes in SW MO and SE Kansas. My heart just wasn't there.
Then, I found a house north of Wichita. It looked promising. I made an offer. It was accepted. Then, I took a long hard look at the rest of the photos and realized it was going to take too much money to repair. Not the $5000 estimated, but closer to $20,000 just to get it re-sided and the wiring brought up to par. I declined the offer.
What to do? I needed to be marketing Condemned to Die: Ask me how. Tell me why. I was up a stump and didn't know how to move forward with the book. I searched the Internet for an answer. It came.
I now have an excellent team working on getting me trained and knowledgeable before hitting the road in the old motorhome. I'll know how to use a smart phone and even to Twitter before I leave here. I am not that old. I can learn new things. For years, my little Brenna kept telling her mom that I could do all things. I know today she is smiling on me.
I can only say that God put this team together. I appreciate all they are doing to help me spread the word of Brenna's story, that no one else will ever have to go through the journey she traveled. I can't disclose their names to preserve their privacy, but they are doing a great job for me. Thank you so much.
I wanted out of this older home, in a neighborhood where housing is increasingly being sold to investors. But, where to go.
Yesterday, I got up and knew that I wanted to see the sun rise again. I wanted to get my future settled.
Tonight, I paced the carport for hours. Then I felt a peace come over me. I knew it would be alright with Brenna if I stayed in Idaho.
Later today, I will go look at a place, 30 years newer than this one, with a fenced in yard for Tippy. I had promised Tippy a yard. She is getting older. Time for Grammie to settle herself down and stop saying, "I'll know where home is when I get there."
The truth is, I have lived in Idaho over 40 years. This is home. I'll start on the book tour next month. I know where I am going and I know this, I'll be back. No more saying, "I'll know where home is when I get there." Home is where the heart is. My heart is with that little girl, but I know that she would be happy for mom to settle here and reach out to happy days again.
While gone, we were in an accident that totalled the pickup and left Brenna with a detached retina in the left eye. That was the beginning of the spiral downhill for her.
My little girl suffered an anoxic brain injury on May 26, 2010. I planned for her to get better. I was still going to take her where she wanted to go. She had chosen a place in Honey Grove, TX to live. It was big enough for rehab equipment and I wanted to have her in a large enough space to teach her to walk again. We had dreams.
Alas, it wasn't meant to be. On October 1, 2011, my little girl died, leaving behind a broken-hearted, restless mother. Without Brenna, I just didn't want to be here. I wanted to move...some place...any place east of here. I didn't really know where I wanted to be, just somewhere but here.
I searched for homes in Oklahoma, to be centrally located in the US, to fly to anywhere I wanted to go. No matter where I contacted a realtor, nothing happened. Realtors either didn't contact me back or I believe they had another agenda on repo homes. I checked out homes in SW MO and SE Kansas. My heart just wasn't there.
Then, I found a house north of Wichita. It looked promising. I made an offer. It was accepted. Then, I took a long hard look at the rest of the photos and realized it was going to take too much money to repair. Not the $5000 estimated, but closer to $20,000 just to get it re-sided and the wiring brought up to par. I declined the offer.
What to do? I needed to be marketing Condemned to Die: Ask me how. Tell me why. I was up a stump and didn't know how to move forward with the book. I searched the Internet for an answer. It came.
I now have an excellent team working on getting me trained and knowledgeable before hitting the road in the old motorhome. I'll know how to use a smart phone and even to Twitter before I leave here. I am not that old. I can learn new things. For years, my little Brenna kept telling her mom that I could do all things. I know today she is smiling on me.
I can only say that God put this team together. I appreciate all they are doing to help me spread the word of Brenna's story, that no one else will ever have to go through the journey she traveled. I can't disclose their names to preserve their privacy, but they are doing a great job for me. Thank you so much.
I wanted out of this older home, in a neighborhood where housing is increasingly being sold to investors. But, where to go.
Yesterday, I got up and knew that I wanted to see the sun rise again. I wanted to get my future settled.
Tonight, I paced the carport for hours. Then I felt a peace come over me. I knew it would be alright with Brenna if I stayed in Idaho.
Later today, I will go look at a place, 30 years newer than this one, with a fenced in yard for Tippy. I had promised Tippy a yard. She is getting older. Time for Grammie to settle herself down and stop saying, "I'll know where home is when I get there."
The truth is, I have lived in Idaho over 40 years. This is home. I'll start on the book tour next month. I know where I am going and I know this, I'll be back. No more saying, "I'll know where home is when I get there." Home is where the heart is. My heart is with that little girl, but I know that she would be happy for mom to settle here and reach out to happy days again.
Sunday, July 29, 2012
Patients and families have rights
I have been reading Head
Cases by Michael Paul Mason. Mason’s book is a compilation and examination
of cases of brain injury.
As I read a chapter about a young man by the name of Rob, I was
struck by a conversation his mother had with staff.
Staff was puzzled as to why they could not get Rob to close his
eyes all the way. Why did he sleep with his eyes half open?
His mother knew the answer. Rob had ALWAYS slept with his eyes
half open.
I remembered when Brenna would not respond when staff ran a
round metal object on the bottom of her foot. They wanted to see her twitch. No
twitch. This gave all the more reason for a willfully uninformed doctor to rule
her in a persistent vegetative state (PVS).
Brenna was not ticklish. She would not have twitched her foot
the day BEFORE her brain injury. She would not have twitched her foot an HOUR before
her brain injury. She just wasn’t ticklish. She never had been. I never knew if
she really wasn’t ticklish or had a strong sense of power over the control of
that ticklish reaction others have.
Brenna had a strong will-power and perhaps in her injured state,
the inner person that knew who she was and what was normal, again resisted the
urge to twitch. She didn’t realize how important it was to play the game, the
only one the doctor knew to play or cared to play.
NO ONE asked me what her normal reactions were before her
injury. No one cared. They came in with their book-learned, pre-assumed ideas,
and made their diagnosis. For all I knew, these doctors could have missed the
day brain injury was discussed in class. For all I knew, they could have graduated
at the bottom of their class.
I call their DX of PVS for Brenna as what it was…pure bunk! I
believe they weren’t qualified to make that determination. One doctor, after
she was dismissed from the first hospital, a doctor who had NEVER seen Brenna,
wrote me a letter to send to her university, giving the DX of PVS. Had he for
ONE moment stepped into her room at the nursing home from hell where he was on
staff, he would have known that Brenna Deshawn Dowd was a living, breathing
human being who KNEW exactly where she was and that the staff there didn’t care
whether she lived or died. Her life made no difference to them. They could
always get someone else to fill the bed.
I was her mother. Brenna was and still is my only beloved child,
the child of my heart. I knew her better than I knew myself. Every doctor
should have asked me what was normal for
Brenna prior to her injury. THEN they might have been able to make an informed
diagnosis. Doctors should make this assessment of all patients with family
members and should pay heed to what they hear.
I believe that making a fully informed diagnosis is outside the
realm of most doctors in modern medicine. The doctors get their MD. In their
opinion I believe that stands for Medical
Divinity. Too many approach the medical profession as if they are on the
fast track to god-head. They make an off-the-wall DX of PVS because they do not
know, care, or understand how to go about it.
A family member who is approached by one of these ghouls should
have every right to see all the credentials of the doctors making the
determination of PVS and brain death. Families should have the right to know
just where this doctor stood in his or her medical class at graduation. Bottom
of the class or in the top 10%? Attendance record? His or her own mental stability? What makes this person an expert? [My 8th grade science teacher, Mr. Schaeve, taught me that an expert was a "drip under pressure".][Others say an expert is someone 50 miles from home.]
Families have a right to know and the medical profession should
have a duty to disclose. We pass laws that require full disclosure on the sale
of a home or a vehicle. We force a garage to stand behind its guarantee. Buy a
house and find a problem that wasn’t disclosed and should have been? Trouble
comes.
Yet, when it comes to the most critical decision of a lifetime,
families are never given full disclosure to the physician’s qualifications to
even care for the patient, much less encourage families to make the tragic
decision to end life, based on a doctor’s possibly ill-informed decision over
quality of life.
Brenna Deshawn Dowd did not die of her brain injury. She died,
in my belief, as the result of a culmination of tragic medical events that led
up to her sudden cardiac arrest (SCA), a list of events that include multiple
hospital and institutional associated infections (MRSA, UTIs, C-Diff,
bloodstream infection, infected gums from 5 broken teeth), improper diabetic protocol for a brittle diabetic, internal
bleeding because doctors refused my request to take her off Coumadin, blood
clots, potassium overload, total disregard for dental care that put infection
from broken teeth into her blood stream, and a general neglect of proper daily care
in all facilities prior to her SCA.
Brenna Deshawn Dowd deserved better than she got from the hands
of doctors in the first 16 months of her brain injury. Only at the end, did she
receive full benefit of a loving, caring staff who gave this mother confidence
that they knew what they were doing. When I saw THEIR tears, my heart eased. They weren't pushing their agendas. They eased this mother's aching heart, knowing the decision that I had to make.
Brenna Deshawn Dowd, your mother has always been so proud of you. I love you forever, forever I do. Always and ever, your Mama loves you.
I want to see the sun rise
I have turned a corner in life. For the first time in months, I awoke early and wanted to see the sun rise. As I stood on the back patio and watched the sun in the eastern sky, God gave me these words.
Lord, I want to See the Sun Rise
By Pamela G. Blaxton-Dowd ©2012
Lord, I want to see the sun rise.
I want to see it with my eyes.
Lord, I want to see your paint brush,
As it colors across the skies.
I want to see it with my eyes.
Lord, I want to see your paint brush,
As it colors across the skies.
I want to see the sun come up,
I want to see it every day.
Lord, I want to see the sun rise,
Show me the colors in your own special way.
I want to see the sun rise,
Oh, bless me on this day.
With the colors of your Heaven
Across my heart each day.
Oh, bless me on this day.
With the colors of your Heaven
Across my heart each day.
Friday, July 27, 2012
Eastward Bound
Plans are moving forward to that day when I will head East
toward Washington, DC. I plan to travel I80 until I get to IA. Then, I head NE
to WI and Northern MI, swinging down through central MI and back to I80. After
leaving Washington, DC, I will make a southern tour, heading back to Idaho.
I will have copies of Condemned to Die: Ask me how. Tell me why.
with me. This is Brenna’s valiant journey to succeed in a medical society that
doomed her to failure. But she showed them. She took her steps. She made her
noises. She even said, “Maum”. Those are cherished memories.
Along the way, I will meet families who daily face the same
struggles I did with Brenna. I plan to video families and hear their stories of
recovery and rehabilitation of patients with a hypoxic-anoxic brain injury.
Congress needs to see faces, needs to hear the success stories.
If no one is tracking HAI patients, then the government needs to change
direction. HAI brains cannot be wasted. HAI patients cannot continue to be
warehoused. We move forward that they might live.
We need change. When I lost my beloved Brenna, I knew that I
must do whatever I could to bring change. To have Congress recognize how
important it is for us to have the same chance at rehabilitation and recovery
as other injuries.
My little girl would not expect her mother to sit quietly with
the knowledge I gained over her 16 months’ fight to win.
For my little Brenna, nothing less than victory.
Wednesday, July 25, 2012
The Rest of the Story
July 25,
2011
One of the WORST days of our misadventure
in an out-of-state facility.
(Comment: This story is NOT in Condemned to Die: Ask me how. Tell
me why. Condemned was written to tell Brenna’s
story.) The facility mentioned in this story can no longer harm my precious daughter. Today, on the
anniversary of this nightmare, I will share with you, “The rest of the story.”
(Thanks Paul Harvey for leaving us this comment.)
Each day as Brenna waited for therapy, her PEG (feeding tube)
was disconnected prior to therapy, usually, sometime around 11 AM. Sometimes, the
PEG would be disconnected for up to an hour before she was wheeled to the
therapy gym. The
scheduled disconnect time for the PEG was no more than two hours each day.
After the best nurse (my opinion) in the facility (and certainly the best to
take care of Brenna) lost her job 10 days into Brenna’s stay, no one else
seemed to monitor that two hour disconnect time.
After Brenna’s therapy sessions, a therapy aide would wheel
Brenna back to her room. From then until 16:30-17:00, no one on staff would
come in to reconnect Brenna to the PEG.
For those of you who do not know, after a PEG tube is
disconnected, the formula hardens in the tube and you can’t just reconnect
without flushing the lines. Many times the call light to Brenna’s room, the
last on the hall, would not work and, since the adjacent room and the one
across the hall were frequently empty, as it was this day, staff was seldom around
that end of the hall to hear a cry for help.
On last July 25th,
the aide brought Brenna back from therapy and left her in her wheelchair. The
room was small and cramped. He forgot to lower the leg rest on her chair.
As I had learned to do in
Boise, I took on the task of reconnecting Brenna’s PEG each afternoon. I
flushed the tube every afternoon, prior to that procedure. This day was
different. I was between Brenna’s chair and the bed. The formula had hardened
and needed to be flushed. I came around her bed to get water. That is when it
happened.
I tripped over the leg rest of
Brenna's wheelchair and hit the door frame to the bathroom. My head split open
and blood was all over the wall and the floor. I don’t know how long I lay on
the floor before I came to enough to look up and see the big dark spots of
blood on the floor.
At first, I didn’t know what
those spots were. Not until I touched them with my fingers and watched more
blood dripping from my head.
I was a long way from Brenna’s
call button. I couldn’t get up. I yelled for help. No one came. No one was
anywhere near that end of the floor. The blood was still dripping from my head.
I remembered my cell phone in
my pocket. I had the cell phone number of the mother of another brain injury
patient down the hall programmed into my phone. I knew she was in the building. I called her to ask her
to get help to me. I closed my eyes.
When I opened my eyes, I could
see faces around me. I didn’t know who they all were, but later learned that
one of them was the Director of Nurses. She ordered the ambulance and chose the
hospital where I was to go.
As I was being wheeled out, my
last concern was addressed to her and the others in the room…“Flush Brenna’s
PEG and get her reconnected.”
I was taken to a downtown Ft.
Worth hospital where began another nightmare. The ER doctor examined me and
sent me for a CT scan. Then I waited. While waiting, I began moving all my
extremities. I wanted to be sure for myself that everything was working. Arms,
legs, fingers, toes…everything was normal.
While waiting to have the wound
stitched, a nurse came in and ordered me to disrobe completely and put on a
hospital gown. Since the problem was with my head, I could not understand why I
needed to have all my clothes off. I told her that I just needed my head
stitched and I didn’t think I needed to have my underwear off for that. She
said it was the doctor’s standard procedure.
I questioned her again. By that
time, the doctor (one I hadn’t seen already and dressed in white) had appeared in
the cubicle and said he thought by then the ER doctor would have told me that I
was being admitted to ICU.
I panicked. My only thought was
getting back to Brenna. My little girl needed me. She didn’t know what happened
to me. She didn’t know where I was. Two little dogs needed me. Who would take
care of them in that Texas heat? The last place I wanted to be was staying
overnight in an ICU ward. He insisted.
He walked around the bed, moving
my extremities, talking fast about my need to be in ICU for observation overnight
and that I couldn’t leave. How could I? My cell phone was dead. I had no idea
where I was. And, I had no way TO leave.
He said I had a hematoma that
would require brain surgery and at least 2-3 weeks in the hospital.
My panic was increasing. I needed
to be with Brenna. I begged to leave. I cried and told him my little girl
needed her mother, that she couldn’t understand. He told me I took the chance
of dying and leaving her anyway.
His patter kept me upset. He
knew it. He was playing a game like the old shell game: keep talking to the audience,
ME, so the nurse wouldn’t know what he was REALLY doing with his hands while
checking my extremities. Quick as a wink, his fast finger invaded an area of my
body that had nothing to do with a brain injury and everything to do with a
physician copping a feel on a helpless patient.
I asked, “Is this what happens
when you come into ER with a head injury if you haven’t seen your own doctor in
months…you get a pelvic?” She never blinked or acknowledged my question.
The ER doctor came in and
stitched my head. He did a great job. At least 12 stitches, underneath and on
the outside of the wound. You can barely see the stitches today. A neurosurgeon
came in to discuss my stay. He did not believe I would need surgery. He assured
me that the stay in ICU was strictly for observational purposes but necessary.
I was taken to ICU where I was
informed that I had missed dinner and the kitchen was closed. Someone brought
me graham crackers and juice. Where do hospitals find this cheap quality food? It felt like cardboard in my mouth
and the juice tasted like a watered
down version of one of those children’s fruit flavored drinks.
When the neurosurgeon came in
to check me before he left for the night, he assured me that if I had no
headaches through the night, I could go home the following morning. He assured
me that absence of any headache or pain, he saw no reason for another CT scan.
During the night, the nightmare
continued. I was periodically awakened for a battery of tests, then the ICU
doctor ordered a CT scan for 3 AM. I refused the CT. I declined the blood tests
at 3 AM. I just wanted out of there. I wanted to be back with Brenna.
Early in the morning, a nurse
came in with my “morning pills”. Since I hadn’t taken a prescription medication
for years, I asked what those were. She said I needed a laxative. WHY! She said
it was because patients who were in a bed for long periods of time needed to
have laxatives.
I had been walking around that
room all night. A laxative!!! I think not! I was so irritated about the
laxative that I don’t remember what the second pill was for. I didn’t take it
either. I just remember it too was for something for the “impending” brain
surgery.
“Brain surgery! The neurosurgeon
assured me I was NOT having brain surgery and I am NOT taking those meds.” (The
surgeon who performed my radical mastectomy years before could attest to my
aversion to unnecessary meds and shots! He had sided with me when a nurse was adamant
about my taking a hypo and I was equally adamant about not taking it.)
The neurosurgeon came in and
told me that he had re-examined my CT scan. He said he believed the small mark
seen on the scan was NOT a hematoma but just a thickening of brain tissue that
happens with getting older. That was a relief. He said the dark spot was so
small, about the size of a pinhead, that even if it were a hematoma, it would
be far more risky to have surgery than to leave it alone and let it heal.
I just wanted to leave that
nightmarish place behind. I wanted to be with Brenna so she wouldn’t worry
about me. I knew I had to be out of there so I could continue to monitor her
care. After he left, I called the mother of the other brain injury patient and
she came to get me from the hospital.
My eye turned black and the cut
gradually healed.
The dogs spent the night at the
Ft. Worth Humane Society.
When I got back to the nursing
home, I just wanted to crawl up beside Brenna, cuddle close to her, and relax.
The blood was cleaned from the floor, but until Brenna was released, a small
amount of blood was still on the door where my head made contact.
At least my nightmare was over.
I told the Director of Nursing about the event in the ER with the doctor’s
wandering fingers. She told me that a pelvic exam was necessary to assess the
extent of any brain damage I might have. Really??? Brenna was 14 months post
her brain injury and she had NEVER had a pelvic as part of the assessment process.
She assured me she would contact someone at the hospital to report it.
After Brenna’s death, I went
online to report the incident to the appropriate agency in Texas. I never heard
back. I contacted lawyers. None were interested.
Forgiving
I had a good day yesterday, sitting with a friend and sharing stories of my Brenna. She told me things that I did not realize Brenna shared with others, the story of Brenna's compassion and ability to forgive.
In Condemned to Die: Ask me how. Tell me why. I talk about Brenna's forgiving nature. She had much to forgive and did. In my heart, I know that she had made her list of people who had wronged her, some deliberately.
Before she became ill, she talked to me about forgiveness. She talked to me about her dad. Their relationship was stretched thin when he passed away in 2004. She remembered his rages at any little thing. No matter how hard she tried to make a difference with him, nothing worked. On the night before he died, I asked him to write a letter to all his children, telling them how proud he was of them. He said he didn't know how. Sadly, the next morning, he quietly died in his sleep, leaving behind at least one broken heart with more questions than answers.
Brenna wanted me to know that she had forgiven her dad. It was important to her that I understood. She listed others and said, "Mom, I forgive them." Such precious words...I forgive.
Too many times we don't know where our children are spiritually, especially when a crisis happens such as happened with my beloved daughter. I grew up in a strong evangelical family. Rules of getting into heaven were strict. I viewed God as rigid, waiting to bop me in the head for anything I did wrong. But that isn't the God I came to know as an adult. That wasn't Brenna's God, not the one she knew.
Her God is loving and compassionate. He teaches us to forgive. He wants us to love others. Brenna loved the down-trodden. She had compassion for those who had little. She lived the life God wanted her to live.
And she forgave, and forgave, and forgave.
I was privileged to be her mother. God honored me with the gift of her life.
Brenna wants everyone to know who her Jesus is.
**********
Read her story, Condemned to Die: Ask me how. Tell me why. The book is available at Amazon, Barnes & Noble, and Westbow Press. Ask your local bookstores to order it for you. Better yet, ask them to carry the book in the store. If you look by author, please look for Pamela G. Blaxton-Dowd.
Thank you and God bless.
In Condemned to Die: Ask me how. Tell me why. I talk about Brenna's forgiving nature. She had much to forgive and did. In my heart, I know that she had made her list of people who had wronged her, some deliberately.
Before she became ill, she talked to me about forgiveness. She talked to me about her dad. Their relationship was stretched thin when he passed away in 2004. She remembered his rages at any little thing. No matter how hard she tried to make a difference with him, nothing worked. On the night before he died, I asked him to write a letter to all his children, telling them how proud he was of them. He said he didn't know how. Sadly, the next morning, he quietly died in his sleep, leaving behind at least one broken heart with more questions than answers.
Brenna wanted me to know that she had forgiven her dad. It was important to her that I understood. She listed others and said, "Mom, I forgive them." Such precious words...I forgive.
Too many times we don't know where our children are spiritually, especially when a crisis happens such as happened with my beloved daughter. I grew up in a strong evangelical family. Rules of getting into heaven were strict. I viewed God as rigid, waiting to bop me in the head for anything I did wrong. But that isn't the God I came to know as an adult. That wasn't Brenna's God, not the one she knew.
Her God is loving and compassionate. He teaches us to forgive. He wants us to love others. Brenna loved the down-trodden. She had compassion for those who had little. She lived the life God wanted her to live.
And she forgave, and forgave, and forgave.
I was privileged to be her mother. God honored me with the gift of her life.
Brenna wants everyone to know who her Jesus is.
**********
Read her story, Condemned to Die: Ask me how. Tell me why. The book is available at Amazon, Barnes & Noble, and Westbow Press. Ask your local bookstores to order it for you. Better yet, ask them to carry the book in the store. If you look by author, please look for Pamela G. Blaxton-Dowd.
Thank you and God bless.
Monday, July 23, 2012
Twitter!!!! Tweet!!! Tweet on Twitter.
Do I ever have a lot to learn!
Twitter!!!! Tweet!!! Tweet on Twitter.
I really am trying at my advanced stage in life to learn new things. Twitter is one of those, but I think I will need a new phone. My $14 ATT phone just isn't going to do the job. And I have not figured out how to get past signing up on Twitter.
I have Brenna's Iphone, smart phone, or whatever it is called. I can't get it to recharge right now. Perhaps being off for 26 months is a good reason it is being stubborn and not charging. I could never figure out the phone before she got sick and now...well, now, her poor old decrepit mother will have to figure it out. With the book tour coming up, I need to have this mastered. Has anyone written a book on Smart Phone for Dummies? Twitter, tweet for Dummies?
I do have a user name on Twitter. While talking to my friend, Virginia, I decided to try CondemnedBrenna, in honor of Brenna's book, Condemned to Die: Ask me how. Tell me why. AND, I will remember that better than some of the suggestions Twitter gave me.
So, for now, the twitter user name is CondemnedBrenna, but I have no clue where to go from here. You can tweet me on twitter and I may twitter back if I ever find my way back to the twitter page. Or maybe I'll just have to be content to flitter.
Door Number One
Today is a time of reflection, a day when I really miss my girl.
I really do miss my best friend, the one person in this world who knew me, who
looked out for me, sometimes a bit misguided, though.
Odd things jog the memory and you think of things you never
dreamed you would think of again. Times of happiness. Times of irritation. And
sometimes, they fall together.
A year or so after my husband died, Brenna began hunting. What
was she hunting? A man. Not one for herself…for her mother. She was looking for
Mom’s “Door Number One”.
Frequently, when we were out, she would glare at me and say, “Mom,
check your 5’oclock.” “Don’t look now, but slowly look behind you.” “Mom. Mom. Door Number One coming at you.”
She actually honed in on one particular person. She said, “He
would make a good dad.”
“Brenna, he IS a dad.”
“Mom, you don’t have to hold back. I like him. I would
approve if you wanted to go out with him.”
“Brenna, your mom is not looking for a man. And, I am certainly
NOT looking for a man who graduated before I was born.”
When she saw the older actresses choosing young men and calling
themselves “cougars”, she thought THAT might be a good choice for me.
“Brenna, I am NOT going
out with anyone who was born after I graduated.”
On a trip east in 2009, we stopped for breakfast at a local
restaurant, somewhere in the hills of Pennsylvania. I saw two men come in and
sit down. Both were in bib overhauls, t-shirts that had obviously seen better
days, Dad was toothless, and both talked with a loud twang.
I smiled at Brenna and said, “Hey, Brenna, slowly look behind
you. There is Door Number One and Door Number Two, one for each of us.”
I didn’t hear that phrase again.
I sure do wish she were here to say it again.
Friday, July 20, 2012
End this term: Persistent Vegetative State
Too easily medical professionals with little qualifications to make a determination of persistent vegetative state (PVS) give families no hope of recovery from an anoxic brain injury. If this ugly term is going to end, it must begin with those of us who have seen miracles, who know our loved ones lived, loved, understood, and fight each day to recover against the doubtful odds the doctors give.
My mind can travel across the country to one success story after another, people for whom doctors gave up. People whose families loved them with a love that would not let them go. Jimmy, Chris, Steve, Jeni, Mack, Sammie, and so many others. They are making it against all odds. But we don't hear their stories in the media. We only hear what the doctors want us to hear.
The British Journal of Medicine published a study in 1996, stating that 43% of patients diagnosed with PVS had been MISDIAGNOSED. That is a whole lot of misdiagnosing. That is a whole lot of families having the rug pulled out from under them and offering them no hope. Many of those diagnosed with PVS were blind or had a severe visual handicap: therefore, they were written off as PVS.
Read the study results here.
The Royal College of Physicians' report on the permanent
vegetative state3
supports the view expressed by others that the diagnosis requires regular
assessment and taking into account the observations by carers and family.5 However,even
these conditions can result in misdiagnosis. Childs et al reported that 37% of
patients admitted more than one month after injury with a diagnosis of coma or
persistent vegetative state had some level of awareness.7 In a group of
longer term patients in a nursing home, Tresch et al found that 18% of those
diagnosed as being in the persistent vegetative state were aware of themselves
or their environment.8
Physicians can graduate at the bottom of their medical class and be tossing out this PVS diagnosis as if they actually learned and retained one iota of information on brain injury rehabilitation. We, the families, are intimidated by their pressure. They know they can pressure enough and get us into a box where we believe that the unholy doctors actually know what they are saying and telling us to do.
The British have it right. Doctors are poorly trained to make this diagnosis. We got the train off the track 30 years ago when the American medical profession developed bio-ethics committees to determine who lives and who dies. This is complicated by the introduction of organ transplants from cadavers. This made ending life of those with a brain injury popular. The world followed us over the cliff.
I have no qualms with donations of kidneys and partial liver transplants from living and informed donors. I have a problem with the medical professionals pressuring the poor and insurance disadvantaged into doing the "noble thing" and "letting go" of the patient without giving families the other side of the story. The story of hope and recovery. The story of miracles.
The diagnosis of PVS is just as ugly as other words and phrases that are now considered unacceptable in our society. It is time we take another look, stop listening to those who make a living off of the transplant market, and think for ourselves.
How do we do that?
1) We demand studies in the USA on the diagnosis of PVS, and not using those who were recently diagnosed.
2) We demand studies in the rehabilitation of patients with a hypoxic/anoxic brain injury.
3) Traumatic Brain Injury (TBI) already receives multi-millions of dollars for research and rehabilitation. We don't have to take money from those projects. We demand that some of the money tossed at frills and pork be transferred to hypoxic/anoxic brain injury rehabilitation.
And, we stop using the term persistent vegetative state for our loved ones. And we stop doctors in their tracks from using it in front of our loved ones.
Thursday, July 19, 2012
Media Class
Yesterday I spent an awesome time in class. Brenna would be proud to know that her mom took a class to learn how to deal with media. She always kept telling me that YES, I could learn something new. Nine of us took the class. I learned not only more for my own journey, but about the careers of the others in the room. What an eye opener! It was good to be in the room with that very nice group of people. Thanks, Steve!
We did a practice press conference where Steve gave us a scenario to digest and decide which questions to ask. Two of us were taken from the room and prepared to be the presenters. The rest of us, prepared our questions. When we all came back together, I told Steve the rest of the people were going to be the "legit" reporters and I was going to be the Yahoo Inquirer reporter who was going to be irritating and try to interrupt the train of thought. That was fun!
After the morning session, we went to the studio to practice interviews. I had done this before but that was almost 20 years ago. This time was preparation for working with the big guns in the media. That is a whole different ballgame.
Steve treated us as if we were being grilled by the big interviewers, no holds barred. I know I need that kind of thing because Brenna's story is controversial.
Afterwards, my friend and media advisor, Steve, arranged for a photographer to take professional photos of me to use for the upcoming tour. I was amazed when I looked at them on the camera screen. Grant, the photographer, made me look so young.
Adam took more notes so he could prepare the press releases and other materials I will need for the trip.
It felt good to know I was in the capable hands of experienced people who work one on one with me and not working out of a call center. The gentlemen were prepared, dressed professionally, and treated me with respect.
I like my new friends. They are awesome. Thanks, Steve, Grant, and Adam.
We did a practice press conference where Steve gave us a scenario to digest and decide which questions to ask. Two of us were taken from the room and prepared to be the presenters. The rest of us, prepared our questions. When we all came back together, I told Steve the rest of the people were going to be the "legit" reporters and I was going to be the Yahoo Inquirer reporter who was going to be irritating and try to interrupt the train of thought. That was fun!
After the morning session, we went to the studio to practice interviews. I had done this before but that was almost 20 years ago. This time was preparation for working with the big guns in the media. That is a whole different ballgame.
Steve treated us as if we were being grilled by the big interviewers, no holds barred. I know I need that kind of thing because Brenna's story is controversial.
Afterwards, my friend and media advisor, Steve, arranged for a photographer to take professional photos of me to use for the upcoming tour. I was amazed when I looked at them on the camera screen. Grant, the photographer, made me look so young.
Adam took more notes so he could prepare the press releases and other materials I will need for the trip.
It felt good to know I was in the capable hands of experienced people who work one on one with me and not working out of a call center. The gentlemen were prepared, dressed professionally, and treated me with respect.
I like my new friends. They are awesome. Thanks, Steve, Grant, and Adam.
Sunday, July 15, 2012
America's Shame
Shame on rehab hospitals who refused to give Brenna a chance to recover and benefit from their services. Seventeen hospitals receive federal funds for the rehabilitation of patients with a brain injury. They want only traumatic brain injuries. They have a 35% quota for hypoxic or anoxic brain injuries and want to reduce that number. A reduction in numbers accepted equals fewer beds available for hypoxic/anoxic brain injury patient and a reduction in services to the most vulnerable.
To read Brenna's story, please check out her book: Condemned to Die: Ask me how. Tell me why. You can purchase the book online through Amazon, Barnes & Noble, or WestBow Press. You can purchase a Kindle or Nook version.
To read Brenna's story, please check out her book: Condemned to Die: Ask me how. Tell me why. You can purchase the book online through Amazon, Barnes & Noble, or WestBow Press. You can purchase a Kindle or Nook version.
Cognition
History of Brenna Deshawn Dowd
These
were sent to rehabilitation hospitals along with videos and PowerPoints to show
Brenna’s progress. One rehab hospital called to tell me they don’t DO
evaluations this way. Many of the rehab hospitals are funded by tax dollars yet
do not want to accept a patient with an anoxic or hypoxic brain injury.
•
Day
1 - Has always known her Mom/always tracked Mom
•
Day
1 - Face showed abject fear at negative comments around her
•
Day
1 – Calmed by Mom singing inspirational songs
•
Day
2 – Opened eyes to watch Mom/ Squeezed friend’s hand
•
Day
3 – Startles to loud sound
•
Day
4 – Tracked staff at hospital
•
Day
5 – Nods yes to questions
•
Day
6 – Raised right hand at mom – 2X –
Staff observed
•
Week
2 – Showed fear at new environment
•
Week
2 – Depression at new environment/spiraling backwards
•
Week
2 – Grinding teeth
•
Week
2 – Cried when Mom left for night
•
Week
2 – Banging head to express pain
•
Week
2 – Kicking with right foot
•
Week
3 – Vocalized frustration at environment
•
Week
3 – Expressed pain in abdomen by pressing with right
hand
hand
•
Week
3 – Expressed need to potty by pumping right arm/hand
•
Week
4 – Cried when physician said she “wasn’t going
anywhere”
anywhere”
•
Week
4 – Extreme agitation – neuro storming
•
Week
4 – Raised mom’s hand when told she was “busting out” of
the first nursing home
•
Week
5 – Sitting on side of bed/holding balance
•
Week
5 – Attempts to clean self after bowel movement – pushing
gown and sheets between
leg
•
Week
5 – Tracking staff
•
Week
6 – Potty feeling activated upon sitting up
•
Week
6 – Fighting too small wheel chair
•
Week
6 – Putting legs out of bed
•
Week
7 – Expressed extreme anger with eyes at
being suctioned
by nurse
by nurse
•
Week
8 – Sucking on foam tooth brush
•
Week
9 – Scissoring in bed to escape messy bed
•
Week
9 – Fighting too small cardiac chair
•
Week
11 – Expressed anger at presence of someone she knew
did not belong in her life
did not belong in her life
•
Week
12 – Responded to Dr. Capricchione/Tracking/Watched
intently
intently
•
Week
13 – Watched BSU Bronco game (and all subsequent games)
•
Week
13 – Song “Climb up Sunshine Mountain” brought her out
of situation caused by excessive potassium
of situation caused by excessive potassium
•
Week
13 – Responded to Dr. Ziola/Tracking/Watched intently
•
Week
13 – Understood transferring to new facility
Therapy
Responses (After transfer to LCTV)
•
Transfer to Life Care Treasure Valley Sept 9,
2010
–
Receiving intensive therapies
–
Watching favorite kids’ movies
–
Tracking sounds
–
Smiling at staff
–
Rolls shoulders forward to sit up
–
Crosses legs at ankles
–
Responding to anyone blocking TV – glares
until person moves
–
Moves head back and forth to “wash” face
–
Sticking out tongue on command
–
Turning head on command
–
Opens mouth on command
–
Stands with assistance (needs encouragement
at times)
–
Straightens spine on command
–
Standing in LiteGait
–
Initiated foot movements on treadmill in
LiteGait
–
Moving feet in LiteGait — up to 1000 feet
–
Lifts head to assist aides with
dressing/trachea mist
–
Pushing leg straight against Mom’s leg
–
Shakes head for “no”/Blinks eyes rapidly for
“yes”
–
Answered appropriately: Are bears blue? Are
penguins purple?
–
Ate snow
–
Pointing tongue
–
Remembers homework to stick out tongue at
everyone
–
Strumming of right hand indicates need to
potty
–
Pushing right hand toward crotch indicates
she has pottied
–
Indicates boredom at isolation in room
–
Lost spacey look in good eye
–
Interested in sink-purposeful movement toward
sink
–
Looked around with interest during transfer
to hospital for PEG replacement
–
Attempts to stand before given OK by
therapist
–
Rolls forward to count of 3
–
Assists in turning herself
–
Holds herself in position to count of 10 most
of the time
–
Blinked yes to “Do you want to go to brain
injury hospital?”
Subscribe to:
Posts (Atom)